In the aftermath of the global health crisis caused by COVID-19, researchers are still examining its various impacts on health. One area of focus is the potential link between COVID-19 and high blood pressure. We'll delve into this connection, shedding light on the role of ACE inhibitors, and discussing how the virus may have affected cardiovascular health.
The Role of ACE and COVID-19
Angiotensin-converting enzyme (ACE) is a key player in the renin-angiotensin-aldosterone system (RAAS), a hormone system that regulates blood pressure and fluid balance in our bodies. It converts the hormone angiotensin I into angiotensin II, a potent vasoconstrictor that causes blood vessels to narrow, thus increasing blood pressure.
When the virus binds to ACE2, it may alter the balance between ACE and ACE2 activity. This could potentially interfere with the regulatory mechanisms of blood pressure in the body.
Additionally, ACE inhibitors, a class of medications commonly prescribed for high blood pressure and heart failure, work by blocking the action of ACE. This results in less angiotensin II being produced, leading to blood vessels relaxing and blood pressure lowering. As ACE inhibitors indirectly increase the activity of ACE2, some researchers initially hypothesized that these medications might increase the risk of severe COVID-19.
However, subsequent studies have not supported this theory. Instead, they indicate that ACE inhibitors do not seem to significantly increase the risk of contracting COVID-19 or developing severe symptoms. In fact, some research suggests that these medications might be beneficial for COVID-19 patients with high blood pressure. It's believed that ACE inhibitors could potentially mitigate some of the harmful effects of the virus on the heart and lungs, although more research is needed in this area to draw definitive conclusions.
How COVID-19 Can Impact Blood Pressure and Cardiovascular Health
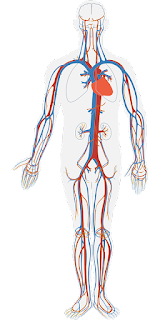
COVID-19, while primarily known as a respiratory illness, can have far-reaching effects on many bodily systems, including the cardiovascular system. It's important to note that while the virus doesn't directly cause high blood pressure, its impact on the body can lead to conditions that may affect blood pressure and overall cardiovascular health.
Breathing Difficulties
COVID-19, a respiratory illness, primarily assaults the lungs, instigating inflammation and damage that can result in significant breathing challenges. The body's reaction to diminished oxygen levels in the bloodstream is to augment the heart rate, thereby facilitating an increased blood flow, and consequently, more oxygen is transported to the various organs. This heightened cardiac activity could potentially escalate blood pressure levels.In an attempt to compensate for the reduced oxygen, the body's respiratory rate might also increase, leading to feelings of breathlessness. The situation is further complicated as the inflamed and damaged lung tissue struggles to effectively exchange carbon dioxide and oxygen. Over time, this persistent low oxygen level can trigger additional symptoms such as confusion or loss of consciousness, owing to the brain not receiving sufficient oxygen.
Furthermore, the increased heart rate and blood pressure place a burden on the cardiovascular system, which can sometimes result in added complications, particularly in individuals with pre-existing heart conditions. This scenario underscores the multi-organ impact of the COVID-19 virus, beyond its primary target - the lungs."
Vascular Changes
The COVID-19 virus triggers an inflammatory response that is not limited to the respiratory system, but extends to blood vessels throughout the body. This inflammation can cause blood vessels to constrict, impairing the smooth flow of blood. Consequently, this can escalate blood pressure as the heart has to work harder to pump blood through these narrowed vessels.Moreover, this inflammatory damage to blood vessels can pave the way for cardiovascular disorders like atherosclerosis. This condition is marked by the accumulation of plaque within the arterial walls, which can cause further elevation in blood pressure and enhance the risk of serious events such as heart attacks or strokes.
In some cases, the inflammation can also cause the inner lining of the blood vessels, or endothelium, to become dysfunctional. This endothelial dysfunction can disrupt the balance of clotting factors, potentially leading to the formation of blood clots. These clots can block blood vessels, further impeding blood flow and exacerbating the cardiovascular strain. This cascade of effects illustrates the broad systemic impact of the COVID-19 virus, extending well beyond its initial entry point in the respiratory system.
Heart Strain
COVID-19 can provoke a condition known as myocarditis, which is essentially the inflammation of the heart muscle, or myocardium. As the heart muscle succumbs to inflammation, its capacity to contract forcefully and rhythmically diminishes, weakening its ability to pump blood throughout the body. This puts extra strain on the heart, as it must work harder to fulfill the body's blood supply demand, resulting in an elevated blood pressure.Moreover, the inflamed heart muscle can also disrupt the normal electrical pathways in the heart, leading to irregular heart rhythms, or arrhythmias. This can further compromise the heart's ability to pump effectively.
In severe cases, if the myocarditis progresses unchecked, the heart muscle can become so damaged and weak that it leads to heart failure. Heart failure represents a serious, life-threatening condition wherein the heart is no longer able to pump enough blood to supply the body's organs with the oxygen and nutrients they require to function properly. This can lead to a cascade of health problems, including fluid buildup in the lungs, fatigue, and ultimately, multi-organ failure if not promptly and properly treated.
Blood Clots
COVID-19 has been linked to a heightened probability of blood clot development. These clots, or thrombi, can lodge themselves in arteries or veins, impeding the free flow of blood. The presence of these obstructions forces the heart to exert more effort to propel the blood past these blockages, resulting in a rise in blood pressure.The relationship between blood clots and high blood pressure is complex and bidirectional. On one hand, the increased pressure can cause damage to the blood vessel walls, which could potentially trigger the formation of more clots. On the other hand, existing clots increase the resistance to blood flow, causing the heart to pump harder and thus raising blood pressure further.
In more extreme circumstances, these blood clots can migrate to critical areas such as the brain or lungs, leading to grave conditions like stroke or pulmonary embolism. A stroke occurs when a clot blocks blood flow to the brain, depriving it of oxygen and nutrients. Pulmonary embolism, on the other hand, happens when a clot lodges in the lungs, hindering oxygen exchange and putting an even greater strain on the heart as it attempts to compensate for the diminished oxygen supply."